Blogs
- All
- Cardiac Sciences
- Clinical Psychology
- Critical Care
- Dentistry
- Dermatology & Cosmetology
- Emergency Medicine
- Endocrinology
- ENT, Neck & Head Surgery
- Gastro Sciences
- General Surgery
- Internal Medicine
- Neuro Sciences
- Obstetrics & Gynaecology
- Onco Care
- Ophthalmology
- Orthopaedics
- Paediatrics
- Plastic Surgery
- Psychiatry
- Pulmonology
- Renal Sciences
- Emergency
- Urology
- Liver Transplant & GI Surgery
- Dietetics & Nutrition
- General
Obstetrics & Gynaecology | Post Date : Jan 17, 2026
A delayed period can instantly trigger worry. Your mind may jump to pregnancy, hormonal problems, or something serious—even when the delay is just a few days. The truth is, menstrual delay is very common and often linked to everyday factors like stress, lifestyle changes, or minor hormonal shifts.
Continue Reading
Internal Medicine | Post Date : Jan 16, 2026
Pine nuts may be small, but they are packed with nutrition and flavor. Often seen in pesto, salads, and gourmet dishes, pine nuts are increasingly becoming popular among health-conscious people.
Continue Reading
Gastro Sciences | Post Date : Jan 16, 2026
Stomach pain is something almost everyone experiences at some point in life. Sometimes it’s just mild discomfort after a heavy meal, and at other times it can be sharp, severe, or worrying. The challenge is that stomach pain (also called abdominal pain) can have many causes—some harmless, some that need medical attention.
Continue Reading
Dietetics & Nutrition | Post Date : Jan 14, 2026
When people talk about weight gain, many assume it’s easy—“just eat more.” But anyone who has tried to gain weight knows it’s not that simple. Eating the wrong foods can lead to fat gain, poor digestion, and low energy, while the right foods help you gain healthy body weight, strength, and stamina.
Continue Reading
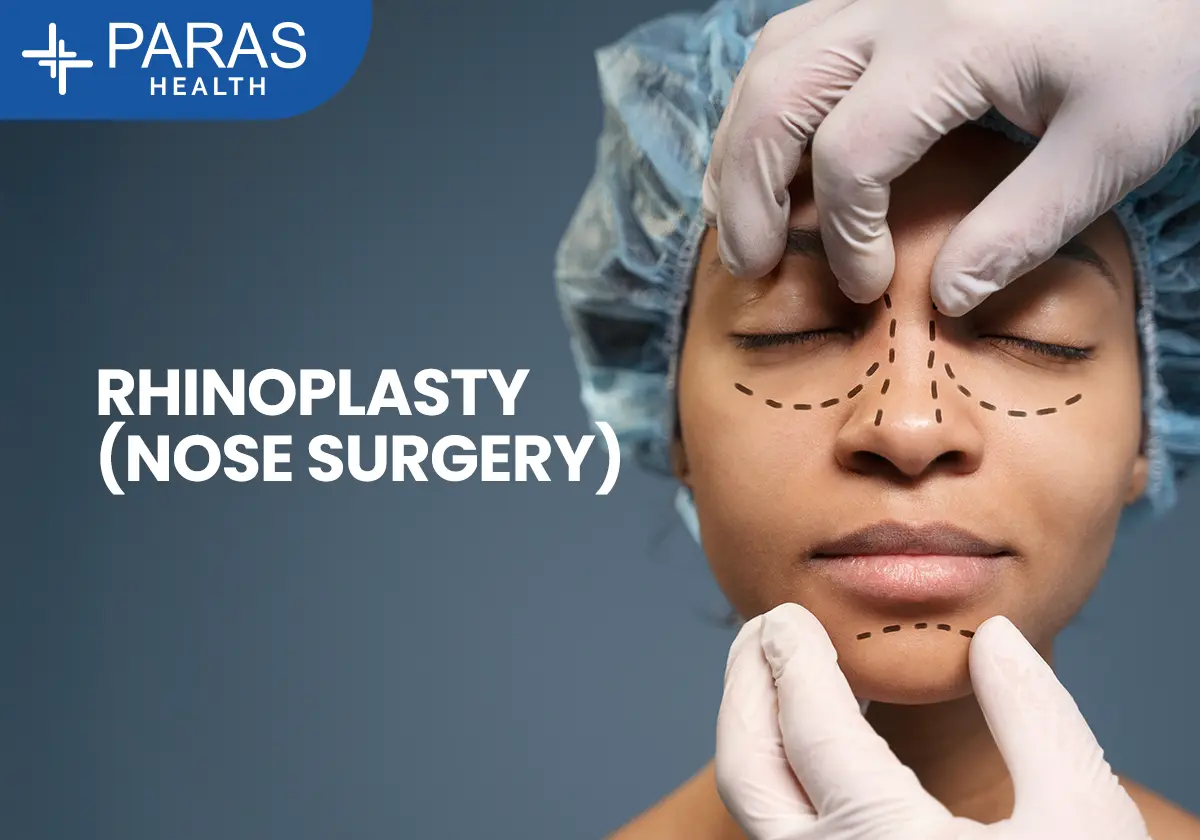
ENT, Neck & Head Surgery | Post Date : Jan 13, 2026
When people hear the term nose surgery, many immediately think of cosmetic changes. But in reality, nose surgery is not just about looks. For thousands of people, it is about breathing better, sleeping peacefully, correcting injuries, and improving quality of life.
Continue Reading
Internal Medicine | Post Date : Jan 08, 2026
Apples are one of the most commonly eaten fruits in the world—and for good reason. They are easy to find, affordable, tasty, and packed with nutrients that support overall health. From improving digestion to supporting heart health and weight loss, apples quietly do a lot for your body.
Continue Reading