Parkinsonism & Overview
Apr 19, 2022
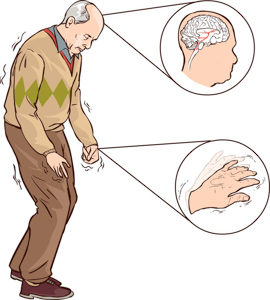
Parkinsonism is a clinical syndrome characterized by tremor, rigidity, bradykinesia & postural instability in varying combinations.
Parkinsonism is an umbrella term under which many different clinical syndromes are present most common being Idiopathic Parkinson’s Disease. Other neurodegenerative atypical parkinsonism syndromes are Multiple system atrophy (MSA), PSP (Progressive Supranuclear Palsy) & Cortical Basal Degeneration.
Idiopathic Parkinson’s Disease –
Most common of all Neurodegenerative Parkinsonism (85%) with an average age of onset (67 years)
Common presenting symptoms are bradykinesia, rigidity, & tremor.
Bradykinesia is a slowness of movements including slow initiation. Rigidity is of cogwheeling type. Tremors are rest tremors that tend to increase with emotional stress & are absent during sleep. These are classic pill-rolling movements started at the distal upper limb usually asymmetric & dampen during an act. Gait instability is a late feature of Idiopathic Parkinson’s Disease; the patient tends to walk with a stooped posture & short stoppage gait (Festinating Gait). There is a loss of associated movements like arm swing. Early gait instability & recurrent falls (within one year of presentation) is usually associated with atypical Parkinsonism.
Non-Motor Symptoms of IPD – loss of Smell, constipation, autonomic dysfunction, urinary hesitancy & incontinence, psychiatric manifestation (hallucination, depression, etc.), & dementia.
Diagnosis – Typical clinical manifestations, lab investigation, DaT Scan (May differentiate IPD & other types of Parkinsonism), routine blood investigation.
Treatment –
- Dopaminergic drugs – Carbidopa-Levodopa Combination – Mainstay of Therapy; Enhances dopamine in Basal Ganglia.
- Anticholinergics – Triphenylhexidine
- Antiviral – Amantadine
- Dopamine Agonist – , Pramipexole, Ropinirole Citrate
These therapeutic remedies are less effective for non-motor symptoms & they should be treated symptomatically.
Multiple System Atrophy – Neurodegenerative disorder manifested by dysautonomia & various combination of Parkinsonism & Ataxia. 2 major forms are:
- MSA – C (Predominantly Cerebellar Feature)
- MSA – P (Predominantly Parkinsonian features)
Mean Age of Onset – 54 year
Signs of Dysautonomia Present – bladder dysfunction, bowel dysfunction, orthostatic hypotension, sexual dysfunction, nocturnal stridor, etc.
Diagnosis –
Tests for Automatic Dysfunction
Presence of Postural Hypotension – Sitting to Standing Drop-in SBP >30 mm of Hg; & diastolic > 15 mm of Hg
MRI Brain – Cruciform Hyperintensity in the pons (T2WI) – Hot cross bun sign
Treatment & Prognosis – No Specified treatment, Parkinsonian features in MSA – P respond to LD; Most patients become wheelchair-bound by 5 years of disease progression.
Mean Survival – 7 to 9 years.
Progressive Supranuclear Palsy (PSP) – First described in 1964; characterized by:
- Vertical Supranuclear Geze palsy
- Axial Rigidity
- Pseudobulbar Palsy
- Mild Dementia
2nd most common Neurodegenerative Parkinsonism:
Age of Onset – 6th – 7th Decade
Typical features – Wide eye stare, furrowing of the forehead with frowning expression (procerus sign), pseudobulbar palsy (dysarthria & dysphagia, emotional incontinence), axial rigidity makes the patient stand in an extended posture. Dementia is associated with frontal lobe dysfunction (executive dysfunction).
Diagnosis: MRI Brain, Mid-brain atrophy present. In the mid-sagittal view, MRI shows atrophy of rostral midbrain, tegmentum, basis pontis & cerebellum (Humming Bird Sign).
Treatment: Dopaminergic agents like levodopa may improve; bradykinesia in about 40% of patients temporarily.
Amitriptyline can be given to control emotional incontinence
Prognosis – Poor quality of life will mean survival of 8 years.
Cortical basal Degeneration – Described in 1967 least common of Atypical Parkinsonism & most asymmetrical; Age of Onset – 60 to 64 years
– Predominantly motor phenomena; asymmetric rigidity, dystonia, myoclonus, apraxia & cortical sensory loss; they may evolve into dementia.
Diagnosis – MRI Brain – Focal Asymmetric Cortical Atrophy with a widening of Sylvian & interhemispheric fissure.
Treatment – No specific treatment. LD is not effective. Benzodiazepines are helpful in myoclonus & Botulinum toxin for dystonia.
Prognosis is poor with reported median survival after onset of about 7 years.

