Managing Parkinson’s Disease: Latest Advances in Care
Mar 04, 2025
Understanding Parkinson’s Disease
Imagine waking up one day and noticing a slight tremor in your hand. At first, it seems like nothing, but over time, movements slow down, balance feels off, and even simple tasks like buttoning a shirt become a challenge. This is the reality for millions of people living with Parkinson’s Disease (PD), a progressive neurological condition that affects movement, coordination, and even mental health.
While there's still no cure, the good news is that researchers are making incredible strides in treatment and care. In this article, we'll dive into some of the latest breakthroughs, surprising symptoms many people don’t talk about, and lifestyle tips that can make a real difference.
What Is Parkinson’s Disease (And Why It’s More Than Just Shaking Hands)?
Parkinson’s disease affects nearly 10 million people worldwide (Parkinson’s Foundation, 2023). It happens when dopamine-producing cells in the brain start breaking down, leading to symptoms like:
One of the biggest misconceptions? It’s not just a movement disorder. Many people experience depression, anxiety, and digestive issues long before they even notice the physical signs. That’s why early diagnosis and personalized care matter more than ever.
What Causes Parkinson’s Disease?
The exact cause is still a mystery, but doctors believe it’s a mix of genetics, environmental factors, and aging. Let’s break it down:
- Genetic Factors
- Around 10-15% of cases run in families.
- Specific gene mutations (LRRK2, SNCA, PARK2, PINK1, and others) have been linked to Parkinson’s.
- If a close family member has Parkinson’s, your risk might be slightly higher, but it doesn’t guarantee you’ll get it.
- Environmental Triggers
- Exposure to toxins: Long-term exposure to pesticides, herbicides, and heavy metals may increase the risk.
- Head injuries: Concussions or repeated trauma to the brain might be a factor.
- Rural living & well water consumption: Some studies suggest these could be linked due to higher exposure to environmental toxins.
- Aging
- Parkinson’s is more common in people over 60.
- As we age, dopamine-producing neurons naturally decline, making the brain more vulnerable.
- Protein Build-up in the Brain
- A protein called alpha-synuclein (which forms Lewy bodies) accumulates in nerve cells, disrupting their function and eventually leading to their death.
Common Symptoms of Parkinson’s Disease
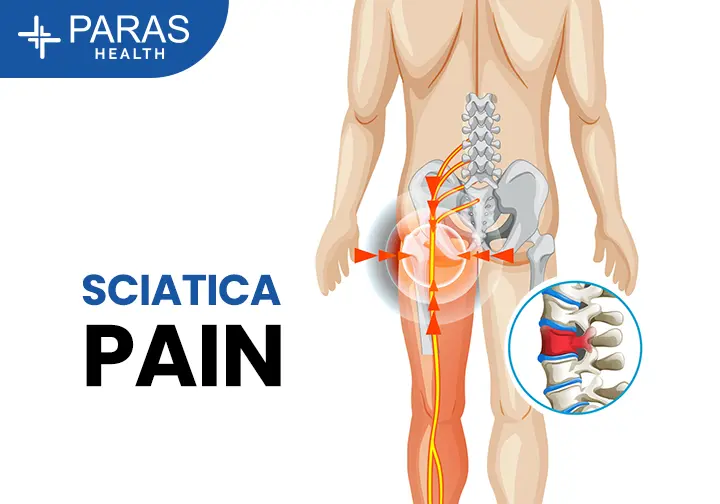
Parkinson’s doesn’t show up suddenly—it starts subtly and gets worse over time. Symptoms can be divided into motor symptoms (affecting movement) and non-motor symptoms.
Motor Symptoms (Movement-Related)
- Tremors: Uncontrollable shaking, often in the hands or fingers, even at rest.
- Bradykinesia (Slowed Movement): Everyday tasks like buttoning a shirt take longer.
- Muscle Stiffness: Tight or rigid muscles that make movement painful.
- Balance Problems: Increased risk of falling due to posture instability.
- Freezing Episodes: Sudden, brief inability to move, especially when walking.
Non-Motor Symptoms (Beyond Movement)
- Cognitive Changes: Memory loss, confusion, and in later stages, dementia.
- Mood Disorders: Depression, anxiety, and apathy are common.
- Sleep Issues: Insomnia, nightmares, restless legs, and excessive daytime sleepiness.
- Loss of Smell: One of the earliest warning signs.
- Constipation & Bladder Problems: Due to nervous system dysfunction.
- Fatigue & Low Blood Pressure: Can lead to dizziness and fainting.
How is Parkinson’s Diagnosed?
There’s no single test for Parkinson’s, which makes early diagnosis tricky. Doctors rely on:
- Medical History & Symptom Assessment
- Neurological Exams: Checking for tremors, muscle stiffness, and movement speed.
- Dopamine Transporter Scan (DaTscan): A specialized brain imaging test that helps confirm dopamine deficiency.
- MRI/CT Scans: Not used to diagnose Parkinson’s directly but to rule out other conditions.
Stages of Parkinson’s Disease
Doctors use the Hoehn & Yahr scale to classify Parkinson’s progression:
- Stage 1: Mild symptoms on one side of the body, barely noticeable.
- Stage 2: Symptoms affect both sides, but daily activities are still manageable.
- Stage 3: Balance and coordination issues become more prominent.
- Stage 4: Severe disability, requiring assistance for movement.
- Stage 5: Total dependence on a caregiver; may need a wheelchair or be bedridden.
How Lifestyle Changes Can Improve Quality of Life
Medical advancements are incredible, but daily habits also play a huge role in managing Parkinson’s.
- Exercise: The Best Medicine?
- High-intensity workouts like boxing, cycling, and tai chi have been proven to slow symptom progression.
- Yoga and stretching improve flexibility, reduce stiffness, and boost balance.
- Speech therapy exercises help maintain a strong, clear voice.
- Eating Right for Parkinson’s
- A Mediterranean diet rich in antioxidants may help protect brain cells.
- High-fiber foods can help prevent constipation, a common struggle for Parkinson’s patients.
- Smart protein timing: Since protein can interfere with Parkinson’s medications, doctors recommend taking them separately from high-protein meals.
- Mental and Emotional Well-being
- Cognitive Behavioral Therapy (CBT) can be a game-changer for managing anxiety and depression.
- Music and dance therapy stimulate brain activity and improve movement control.
- Building a Strong Support System
- Educating family members and caregivers leads to better patient support and improved quality of life.
- Joining support groups and online communities can make the journey less lonely.
Future Treatments & Ongoing Research
Scientists are working on new therapies that may one day slow or stop Parkinson’s progression:
- Stem Cell Therapy: Potentially replacing damaged neurons.
- Gene Therapy: Targeting faulty genes that may contribute to Parkinson’s.
- Neuroprotective Drugs: Testing new medications that could slow disease progression.
- AI & Early Diagnosis: Using artificial intelligence to detect early signs of Parkinson’s.
Expert Parkinson’s Care at Paras Health
Managing Parkinson’s requires specialized care and a team-based approach. At Paras Health, our experienced neurologists, physiotherapists, and rehabilitation specialists provide personalized treatment plans tailored to each patient’s needs, using the latest advancements in Parkinson’s management.
Don’t wait—take control of your health today! Call us at 8080808069 or book an appointment now to consult with our experts.
Frequently Asked Questions (FAQs)
What are the first signs of Parkinson’s disease?
The early signs can be subtle and often mistaken for normal aging. These may include a mild tremor in one hand, slower movements, changes in handwriting, loss of smell, and sleep disturbances. Some people also notice stiffness that doesn’t go away with movement.
Is Parkinson’s disease hereditary?
Most cases of Parkinson’s are not directly inherited, but having a family member with the condition may slightly increase the risk. Researchers are still studying genetic links to better understand the hereditary factors.
Can lifestyle changes slow Parkinson’s progression?
Yes! Regular exercise, a healthy diet, staying mentally active, and maintaining a strong social network can all help slow the progression of symptoms and improve quality of life.
Are there any new treatments for Parkinson’s?
Yes, exciting advancements like gene therapy, stem cell research, new medications, and AI-powered personalized treatments are showing promise in improving symptom management and slowing disease progression.
Does Parkinson’s affect only movement?
No, Parkinson’s also affects mood, sleep, digestion, cognition, and even speech. Many patients experience anxiety, depression, and memory issues along with motor symptoms.
Can Parkinson’s patients live a normal life?
With the right treatment, exercise, and support, many people with Parkinson’s continue to live fulfilling lives for years. Early diagnosis and proactive management are key to maintaining independence.